According to the National Alliance on Mental Illness (CDC), one in five U.S. adults experienced mental illness in 2024.
Data also shows that Americans’ sexual health is not optimal, with one in five Americans having a sexually transmitted infection (STI), and about 43% of women and 31% of men experiencing some form of sexual dysfunction.
These healthcare trends are not mutually exclusive. “Mental health and sexual health are closely interconnected and can significantly impact each other,” says William Hernandez, APRN, ANP-BC, PMHNP-BC, a nurse practitioner at Q Care Plus.
Will, whose clinical work has focused on marginalized patient communities, with specialties in HIV prevention and treatment and caring for unrecognized mental health conditions, began his career in LA County’s emergency and trauma departments. He later left the ED and moved to primary care, which he describes as “trading off immediate, life-threatening events for quieter and more constant, smoldering assaults on well-being.” In addition to his intimate familiarity with the impact of the social determinants of health, Will recognizes the importance of mental health in successfully addressing other wellness concerns, including sexual health. Read on for his discussion with The Avita Blog about the link between sexual and mental health, why building strong relationships is crucial to both, and how to find healthcare providers who aren’t afraid to talk about it.
Avita: Most readers have a general idea of what mental health is (defined as “the component of behavioral health that includes our emotional, psychological, and social well-being”). However, not everyone may be familiar with the term sexual health. How would you define it?
Will Hernandez, APRN, ANP-BC, PMHNP-BC, nurse practitioner at Q Care Plus:
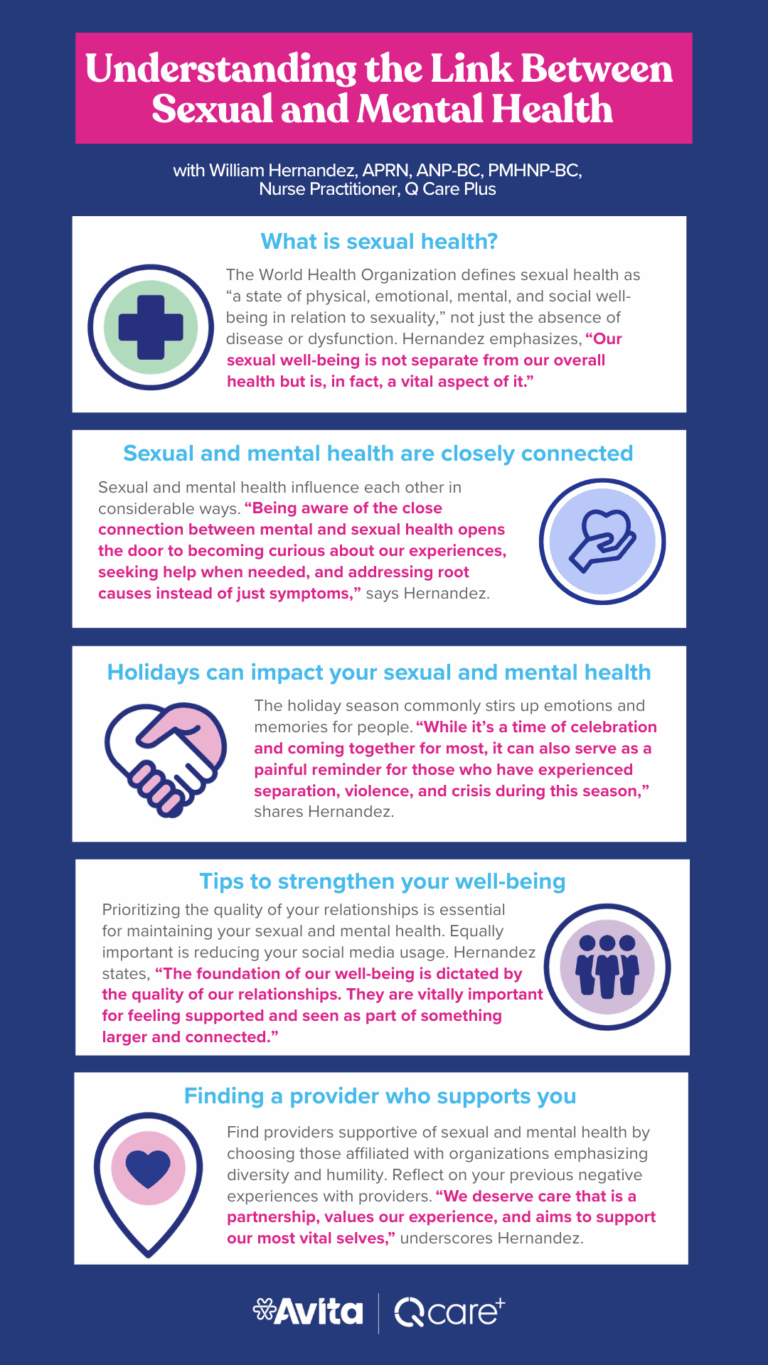
I’m a big fan of the World Health Organization’s definition. They describe sexual health as “a state of physical, emotional, mental, and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction, or infirmity.” I like how their definition is expansive and inclusive of all aspects of who we are. It clarifies that our sexual well-being is not separate from our overall health but is, in fact, a vital aspect of it. It makes me reflect on both our inner experience of health and how the systems around us can support or hinder it.
Being aware of the close connection between mental and sexual health opens the door to becoming curious about our experiences, seeking help when needed, and addressing root causes instead of just symptoms.
Will Hernandez, APRN, ANP-BC, PMHNP-BC
Nurse Practitioner, Q Care Plus
Avita: Are specific marginalized populations (for example, members of the LGBTQ+ community or people living with chronic diseases like HIV) more likely to experience issues with their sexual and mental health? If so, why?
Will: Living on the margins comes with its own set of difficulties and realities that stack the odds against living our most vital lives. Adding insult to injury, we know that they have additive effects. Living on the margins with a chronic health condition has the compounded potential to affect us negatively.
An issue not to be missed is the impact of stigma related to HIV and mental health conditions. While we’ve come a long way in recognizing HIV as a chronic, manageable health condition with safe and effective treatment options that, when properly followed, prevent the transmission of infection, more education and conversations are needed.
Regarding mental health conditions, we still have a long way to go in effectively communicating what these experiences are, what they truly mean, and how to access support and care. We’re making progress overall, but we must support each other to keep moving forward.
Living on the margins comes with its own set of difficulties and realities that stack the odds against living our most vital lives. Living on the margins with a chronic health condition has the compounded potential to affect us negatively.
Will Hernandez, APRN, ANP-BC, PMHNP-BC
Nurse Practitioner, Q Care Plus
Avita: We’re coming up on the holidays. Is this a particularly vulnerable time for people when it comes to sexual and mental health? If so, why?
Will: The holiday season commonly stirs up many emotions and memories for us. While it’s a time of celebration and coming together for most, the holidays can also serve as a painful reminder for those of us who have experienced separation, violence, and crisis during this season. Some of us may find this time of collective coming together as just the opposite — a time of absolute loneliness and abandonment.
Seeking contact, whether that’s calling a friend, dialing a support line, hitting the bar, or hooking up more often, is an attempt at connection. If any of these options start to feel problematic or cause negative, unintended consequences, taking a moment to pause is warranted. Perhaps it’s time to explore what our real needs are and search for alternative ways to meet them.
While it’s a time of celebration and coming together for most, the holidays can also serve as a painful reminder for those of us who have experienced separation, violence, and crisis during this season. Some of us may find this time of collective coming together as just the opposite — a time of absolute loneliness and abandonment.
Will Hernandez, APRN, ANP-BC, PMHNP-BC
Nurse Practitioner, Q Care Plus
Avita: What are your top tips for strengthening mental health and sexual health?
Will: That’s very simple: focus on the quality of your relationships. It’s a straightforward answer, but it can be complex for some of us. We know that the foundation of our well-being, which includes most dimensions of our experience, is dictated by the quality of our relationships, whether with relatives, close friends, chosen families, communities of affinity, or professional coworkers. These relationships are all vital for feeling supported and recognized as part of something larger and connected.
Giving yourself some space from social media is a close second.
Avita: Many people feel uncomfortable discussing their sexual and mental health or have had negative experiences doing so with a previous provider. Do you have any tips for finding a healthcare provider who welcomes open, holistic conversations about sexual and mental health?
Will: Look for healthcare organizations that prioritize and champion the benefits of diversity and humility in their visions and missions. Generally, you will find healthcare providers who have been attracted to practicing in these environments because of the alignment of personal conviction with organizational vision.
I also encourage folks to reflect on their past negative experiences with providers. What about the encounter stands out? How did you know that something was off? We want to become clear in our knowing and trust it. We deserve care that is a partnership, values our experience, and aims to support our most vital selves.
We deserve care that is a partnership, values our experience, and aims to support our most vital selves.
Will Hernandez, APRN, ANP-BC, PMHNP-BC
Nurse Practitioner, Q Care Plus